Head and Heart
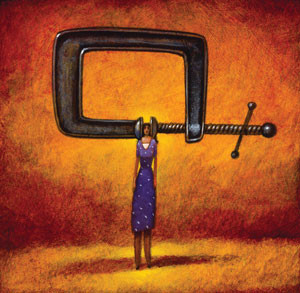
Beyond pain: Migraines have been linked to higher cardiovascular disease risk.
by Susan Weiner, Energy Times
The French have a saying that translates as “the heart is forever making the head its fool.” For those who endure migraines, the opposite may be true: Migraine sufferers are slightly more prone to heart attacks and other cardiovascular ills than others.
 According to the National Headache Foundation (NHF, www.headaches.org), 70% of the more than 29 million Americans with migraine are women; fluctuating estrogen levels may be the reason. While the precise cause of migraines is not fully understood, swelling of blood vessels in the brain can trigger throbbing pain in the eye, jaw or face, sensitivity to light and sound, and nausea and vomiting. Stress, lack of food or sleep, anxiety, weather changes and certain foods can set off an attack.
According to the National Headache Foundation (NHF, www.headaches.org), 70% of the more than 29 million Americans with migraine are women; fluctuating estrogen levels may be the reason. While the precise cause of migraines is not fully understood, swelling of blood vessels in the brain can trigger throbbing pain in the eye, jaw or face, sensitivity to light and sound, and nausea and vomiting. Stress, lack of food or sleep, anxiety, weather changes and certain foods can set off an attack.
Visual disturbances known as aura—such as partial blindness or seeing flashing lights—that may accompany migraine appear to be especially problematic. Among women 45 and older who experience aura, the risk of dying from heart attack, stroke and heart disease is twice that of women without migraine (BMJ 8/24/10 online).
People with migraine were found to be twice as likely to experience heart attack, diabetes or a heart abnormality; aura pushed risk to the highest levels (Neurology 2/23/10).
However, the threat posed by migraines is not as great as that of other risk factors. “Being twice as likely to have a heart attack translates into 4.1% of people with migraine compared with 1.9% of those without, which is not that much of an increase in real numbers,” explains Carolyn Dean, MD, ND, author of The Magnesium Miracle (Ballantine; www.drcarolyndean.com).
Most migraine sufferers would tell you that reducing the risk of an attack is a worthy goal of its own. In one NHF survey, nine out of 10 reported not being able to function normally when a migraine strikes.
Life-Altering Headaches
Jodie Pulkinen knows how migraines can disrupt one’s existence. To relieve the pain she has hidden in dark rooms, driven to the emergency room for shots of Demerol and ingested enough ibuprofen to cause liver damage. She’s also struggled with a heart condition marked by chest pain, fatigue, rapid heart rate and palpitations.
In 2004, Pulkinen’s resting heart rate stayed at the very high 220 beats per minute for several hours. Soon after she underwent a mitral valve catheter ablation, a procedure that fixed her heart and unexpectedly lessened her migraines. “I never thought the migraines and the heart condition were connected,” says Pulkinen, 43, a project coordinator for the American Lung Association in Burdett, New York. “After the surgery, I had fewer headaches. If I’d known, I could have done something about my heart a long time ago.”
After the surgery Pulkinen made dietary changes. “I cut out all caffeine,” she says. “No coffee, no soda, no chocolate. I’ve reduced my sugar intake as well.” Migraine sufferers should also avoid an amino acid byproduct called tyramine, found in a number of foods and food additives including MSG, aged cheese, sauerkraut, alcohol and preserved meats. Eating cold foods can trigger migraines, as can skipping meals and becoming dehydrated. In addition, extra body fat has been found to both provoke migraines and increase heart risk.
Taking a magnesium supplement and eating magnesium-rich foods such as green vegetables and whole grains can not only fend off migraines but also help maintain a steady heart rhythm and lower blood pressure. This mineral, which prevents blood vessel spasms and regulates pain receptors, has been shown to help ease migraine (Magnesium Research 6/08). “A deficiency in magnesium will cause migraines and heart disease. Treating with magnesium can treat both,” says Dean.
Relaxing for Relief
Migraines and heart disease run in the family of Andrew Levy, PhD. In addition to taking blood pressure medication that eases migraines, Levy, an English professor at Butler University in Indianapolis and author of A Brain Wider Than The Sky: A Migraine Diary (Simon & Schuster), eats less, exercises more and practices stress reduction. “The fact that doctors have told me about these potential links between heart disease and migraine has actually not been a source of stress for me,” says Levy. “It has helped me to understand my own body better from a holistic standpoint.”
As Levy has discovered, learning how to relax is a key to reducing migraines. In one study, a combination of gentle yoga postures and breathing exercises lessened migraine frequency and pain, and improved mood (Headache 5/07).
Migraine sufferers can also benefit from the herb feverfew, which slows the production of inflammatory compounds and helps maintain proper vessel tone. A combination of folic acid, vitamin B6 and vitamin B12 may reduce migraine frequency and lower levels of homocysteine, an amino acid linked to coronary disease and migraines (Pharmacogenetics and Genomics 6/09). CoQ10, a supplement best known for its cardiac benefits, may help reduce migraine frequency.
If your migraines persist, see a practitioner and don’t assume the worst. As Aristotle once wrote, “Educating the mind without educating the heart is no education at all.”
When It Isn’t a Migraine
It’s hard to find an adult who hasn’t had a headache at least occasionally. But for some people headaches are, if not a daily occurrence, frequent enough to interfere with their quality of life. Besides migraine, the National Headache Foundation classifies chronic headache into the following categories:
- Cluster: Described as even more severe than migraines, these headaches occur in groups and with little warning for weeks or months before disappearing for months or years. They tend to strike late at night or in the morning. Most sufferers are men, and both smoking and alcohol use are precipitating factors.
- Hormone: These headaches can occur as part of premenstrual syndrome (PMS) or accompany the menstrual period itself; some women may experience hormonal headaches as they pass through menopause. Pregnancy usually brings relief from migraines because hormones don’t fluctuate the way they usually do during a woman’s menstrual cycle. Migraines that do occur during pregnancy tend to strike in the first trimester.
- Rebound: Headaches triggered by the over-use of medications, particularly those that contain caffeine.
- Sinus: Headaches triggered by infection, inflammation or other problems with the sinuses. Symptoms include a dull ache in the forehead or behind the cheekbones and a sense of sinus fullness.
- Tension: Most headaches that occur every once in a while fall into this category, but some people experience tension headaches on a chronic basis. More annoying than throbbing, these headaches are often centered in the forehead, temples or back of the head and the neck; some people feel as though a band is being tightened around the head. Chronic tension headache can stem from physical causes—poor posture or lighting, eyestrain, misalignments of the jaws or teeth, spinal problems involving the neck—or emotional ones such as anxiety or depression.
A sudden, severe headache can signal the occurrence of a stroke; such headaches are medical emergencies, especially if accompanied by a sudden lack of balance, difficulty speaking and/or weakness on one side of the body. A relatively small number of headaches can stem from other organic causes such a brain tumors or infections, or other serious—but fortunately rare—conditions.
If you suffer from frequent headaches, try keeping a pain diary: when the pain starts, the nature of the pain (throbbing, dull, piercing) and where it occurs, any other symptoms and what you took for relief. If you can see a pattern, trying also keeping a food diary as well—sometimes a simple change in diet can do the trick. Some people find relief through acupuncture, massage and other kinds of bodywork. If your headaches are stress-related, make your you get adequate supplies of vitamin B and both calcium andmagnesium, which are available in combination supplement form; the herb white willow bark may also help.